For decades, medical science and people believed that Parkinson’s disease originated in the brain, primarily affecting motor function in the body due to loss of dopamine-producing neurons. However, now that science and research are continually advancing, it is challenging the idea that the starting point can likely be: “The gut.”In a landmark study published in NPJ Parkinson’s disease, scientists conducted a global research and meta-analysis on gut microbiota and uncovered consistent microbial, metabolic and functional changes in the people with Parkinsons.Let’s get into how Parkinson’s might start in the gut.
What is Parkinson’s disease

The study explains that Parkinson’s is a neurodegenerative disease and it impacts the nervous system of our bodies. It makes the neurons of our brains weaker, and they are damaged gradually. As parkinson’s continues to move forward with time, individuals suffering from it might find it hard to walk, speak or perform everyday activities. Even though a number of brain areas are involved in Parkinson’s disease, the most frequent symptoms arise from the degeneration of neurons within an area at the base of the brain known as the substantia nigraOne of the brain regions most impacted by the disease is the Substantia nigra, a region which manufactures dopamine, the neurotransmitter that transmits signals towards more smoother brain function and goal-oriented movement. Research indicates that the majority of PD individuals have lost 60 to 80% or more of their cells in the substantia nigra that produce dopamine at the time of symptom onset.
Most commonly occurring symptoms of Parkinson’s disease
- Tremor (shaking)
- Muscle stiffness (resistance to movements)
- Postural instability (lack of balance)
- Bradykinesia (the slowing down of spontaneous movements)
In addition to the characteristic symptoms, people with PD may experience other problems as well:
- Mental and emotional health problems, such as anxiety or depression
- Difficulty in swallowing and chewing
- Changes in speech (too slurred or too quick)
- Urinary problems (changes in bowel movements or bladder control)
- Common sleep disorders such as insomnia, nightmares, and restless sleep
- Cognitive problems such as slowed thinking, visuospatial skills, language and reasoning problems and even dementia
How does the GUT come into play in all of this
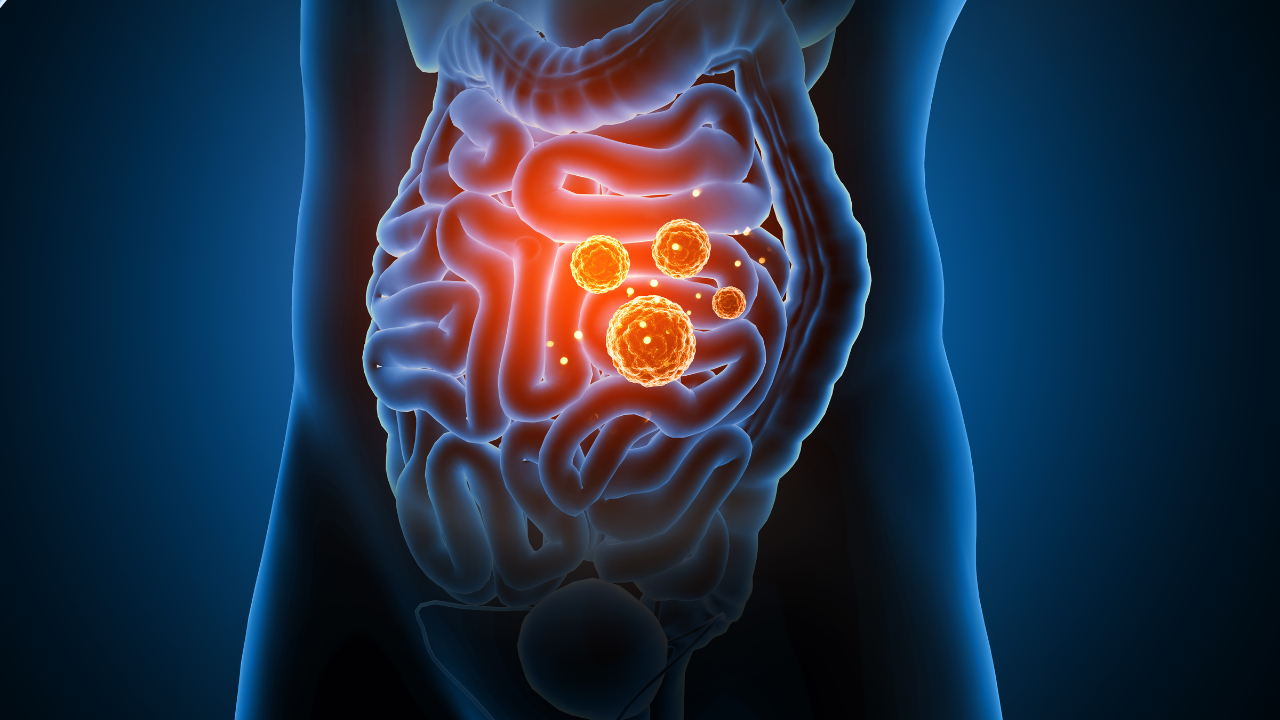
In an effort to understand the Gut and parkinson’s disease connection better, researchers conducted a comprehensive meta-analysis using shotgun and metagenomic sequencing data.The study was conducted using stool samples from 94 individuals who were diagnosed with Idopathic PD (From Japan) and 73 samples of absolutely healthy people.To further broaden the scope of study, people from USA, Germany, China and Taiwan were also looped in, creating a global pool of over 800 people, affected by PD and 550 others who were healthy.What the study revealed was absolutely shocking. The consistent changes in the gut microbiome of people who suffered from Parkinson’s across all populations, of major finding was that people with PD had higher microbial diversity, meaning, there was a more even distribution of bacterial species in the gut as compared to healthy individuals.Furthermore, the people with PD showed a dramatic decline in genes involved in vital nutrient production. Genes such as riboflavin and biotin (Vitamin B2 and B7, respectively) were significantly low across all datasets. The abundance of carbohydrate-active enzymes (CAZymes), which help microbes break down and utilize complex carbohydrates, was also markedly lower in the PD group, all of which are likely to impair gut barrier function, as many of the associated vitamins and metabolites are involved in maintaining the integrity of intestinal lining.
The results suggest a stronger connection between the gut-brain axis

The research suggests that the deterioration of key microbial functions, especially those that support the gut barrier and protect the internal gut lining, could allow harmful proteins such as misfolded alpha-synuclein to emerge in the intestinal nervous system and travel to the brain via the vagus nerve. it not only highlights the gut microbiome as the potential contributor to PD but also a promising target for early detection, prevention and intervention.